Listeria Outbreak Prompts Nationwide Deli Meat Recall, What to Know
- The U.S. Department of Agriculture Food Safety and Inspection Service (FSIS) announced a recall of over 200,000 pounds of Boar’s Head products on July 26 amid a Listeria outbreak.
- Deli meats sliced at the counter have been linked to the outbreak, which led to two deaths and 28 hospitalizations, according to the CDC.
- You should avoid unheated deli meat if you are pregnant, age 65 or older, or have a weakened immune system.
The U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) announced a nationwide recall of Boar’s Head deli meats on July 26 that may be contaminated with Listeria monocytogenes.
The recall includes 207,528 pounds of Boar’s Head liverwurst and other deli meat products.
A widespread Listeria outbreak in the United States has resulted in two deaths and 28 hospitalizations across 12 states.
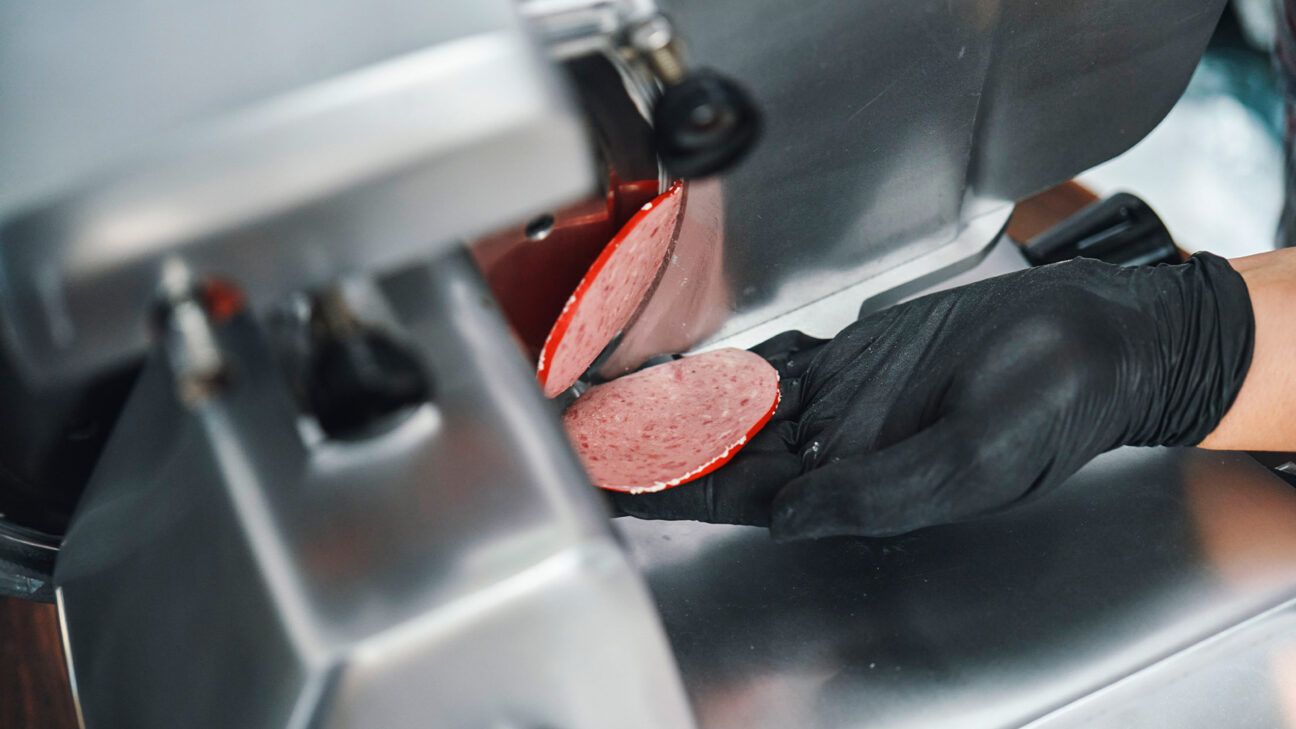
The outbreak has been linked to meat sliced at deli counters, not prepackaged deli meats, according to a July 2024 investigation notice from the Centers for Disease Control and Prevention (CDC).
The CDC warns that Listeria is a bacteria that causes a foodborne illness called listeriosis, which is particularly dangerous for pregnant people and other high risk groups.
The affected individuals span from the Midwest to the East Coast, with lab samples collected between May 29 and July 5. In interviews, most people reported eating deli-sliced meats, particularly turkey, liverwurst, and ham.
Despite the Boar’s Head recall, the CDC’s investigation into this outbreak is ongoing to determine whether other products sliced or prepared at delis are contaminated with Listeria.
Who is most at risk after Listeria exposure?
Dr. Brian Labus, PhD, MPH, an assistant professor in the Department of Epidemiology and Biostatistics, School of Public Health, University of Nevada Las Vegas, cautioned that certain individuals face a higher risk of severe illness from Listeria.
He told Healthline that while most people consuming contaminated food may experience mild gastrointestinal symptoms that resolve quickly without treatment, high risk groups are particularly vulnerable.
Populations at high risk for serious Listeria infections include:
- pregnant people and newborns
- individuals aged 65 or older
- those with weakened immune systems
Symptoms typically appear within two weeks of consuming contaminated food but can manifest as soon as the same day or as late as 10 weeks later.
Labus said pregnant people who contract the bacteria “often have a very mild illness,” such as fever, muscle aches, or tiredness, “but that illness can lead to [pregnancy loss], premature delivery, or serious [life threatening] infections of the newborn.”
Non-pregnant individuals may also experience fever, muscle aches, and tiredness, along with additional symptoms like headaches and confusion, according to the CDC.
Labus warns that older adults and people with weakened immune systems can develop dangerous Listeria infections that enter the bloodstream or brain.
This is “a very serious invasive infection that usually requires hospitalization and kills about one out of every six people infected [with invasive listeriosis],” he said.
Why is deli meat causing listeria
Deli meats sliced at the counter carry a higher risk of bacterial contamination, like Listeria, compared to pre-packaged deli meats.
“The difference is the risk of cross-contamination,” said Labus.
He explained that while both types of deli meats can arrive from the manufacturer already contaminated with Listeria, pre-packaged options minimize this risk by avoiding direct contact with other products.
Slicing meats at the deli can transfer Listeria from contaminated meats to other foods. Equipment and surfaces used for slicing can harbor bacteria, causing contamination of other items prepared in the same area. This significantly raises the risk of bacteria being present in deli counter food products.
“This is why it is so important that we keep Listeria from entering these foods in the first place,” Labus stressed, emphasizing the need for vigilance in food manufacturing and handling practices.
If you suspect that you have purchased any deli products that may be contaminated, throw them away immediately to ensure your safety and well-being.
Is it safe to eat meat from the deli?
According to Labus, consumers face challenges when purchasing deli meats because there are no visible signs of Listeria or other foodborne pathogens. “This is why we have a robust food protection system in the country,” he said.
He explains that the food industry and regulators collaborate to ensure that food is prepared and handled safely, including a zero-tolerance policy for Listeria in the food supply.
Labus said the problem is that Listeria “thrives in low-temperature, high-salt conditions — the exact conditions we generally use to prevent bacterial growth in food.” In other words, refrigeration doesn’t prevent or kill Listeria.
So, for those at higher risk of severe illness, such as pregnant women, the CDC recommends avoiding deli meats altogether or heating them to an internal temperature of 165°F or until steaming hot before consumption.
Additionally, ready-to-eat products like deli salads, soft cheeses, and cut melons can also become contaminated with Listeria.
Therefore, the CDC advises high risk individuals to choose safer foods, such as:
- heated meats
- hard cheeses
- homemade deli-style salads (potato, tuna, chicken)
- fresh melon and other fruit cut at home
Is sliced deli meat healthy?
Kiran Campbell, RDN, a registered dietitian nutritionist and medical nutrition advisor at Dietitian Insights, explained that deli meats are considered ultra-processed foods.
“While not all ultra-processed items are harmful,” she noted, ultra-processed meats may indeed pose health risks.
Processed deli meats tend to be high in sodium, saturated fat, and preservatives, contributing to issues like heart disease, diabetes, and certain cancers, she said.
Campbell also highlighted that the World Health Organization (WHO) classified processed meats as Group 1 carcinogens, meaning there is convincing evidence that processed meats cause cancer in humans.
Every 50 grams of processed meat consumed daily might increase colorectal cancer risk by about 18%.
If you decide to eat deli meats, Campbell advised choosing single-source options like sliced chicken, turkey breast, or roast beef instead of varieties like bologna, salami, and head cheese that contain mixed meats and animal byproducts.
She also recommends selecting:
- minimally processed deli meats with fewer additives
- products lower in sodium and saturated fat
- organic and grass-fed options, which may be more nutritionally dense
- meats raised without antibiotics
- options without added nitrites or nitrates, often labeled “uncured”
However, uncured meats typically use ingredients like celery powder, which still contain natural nitrates. It’s unclear if natural nitrites are actually safer.
Ultimately, while it may take more effort, cooking and cutting lean meats at home is usually the safest and healthiest option for sliced meats.
Takeaway
A multi-state Listeria outbreak in the United States has resulted in 2 deaths and 28 reported illnesses in July 2024.
The CDC has linked these cases to deli-sliced meats, but the specific products involved in the outbreak have yet to be identified.
High risk groups — particularly pregnant individuals, people ages 65 or older, or those with weakened immune systems — are advised to either avoid deli-sliced meats altogether or ensure that all deli meats are heated to a high internal temperature of 165°F to kill bacteria before consumption.







