Weight Loss Drugs Like Wegovy and Ozempic Can Influence Taste Sensitivity

- GLP-1 drugs like Ozempic and Wegovy may significantly influence taste perception, a new study finds.
- These drugs may also change how the brain responds to sweet tastes.
- This change may be one of the mechanisms by which these drugs help drive weight loss.
A new study finds that semaglutide (sold under the brand names Ozempic and Wegovy) influences taste sensitivity and how the brain responds to sweet tastes. The scientists also measured changes in gene expression in the tongue related to taste perception.
Study lead, Mojca Jensterle Sever, PhD from the University Medical Centre in Ljubljana, Slovenia presented the results at ENDO 2024 on Saturday, June 1. ENDO is the Endocrine Society’s annual meeting in Boston, MA.
What is semaglutide?
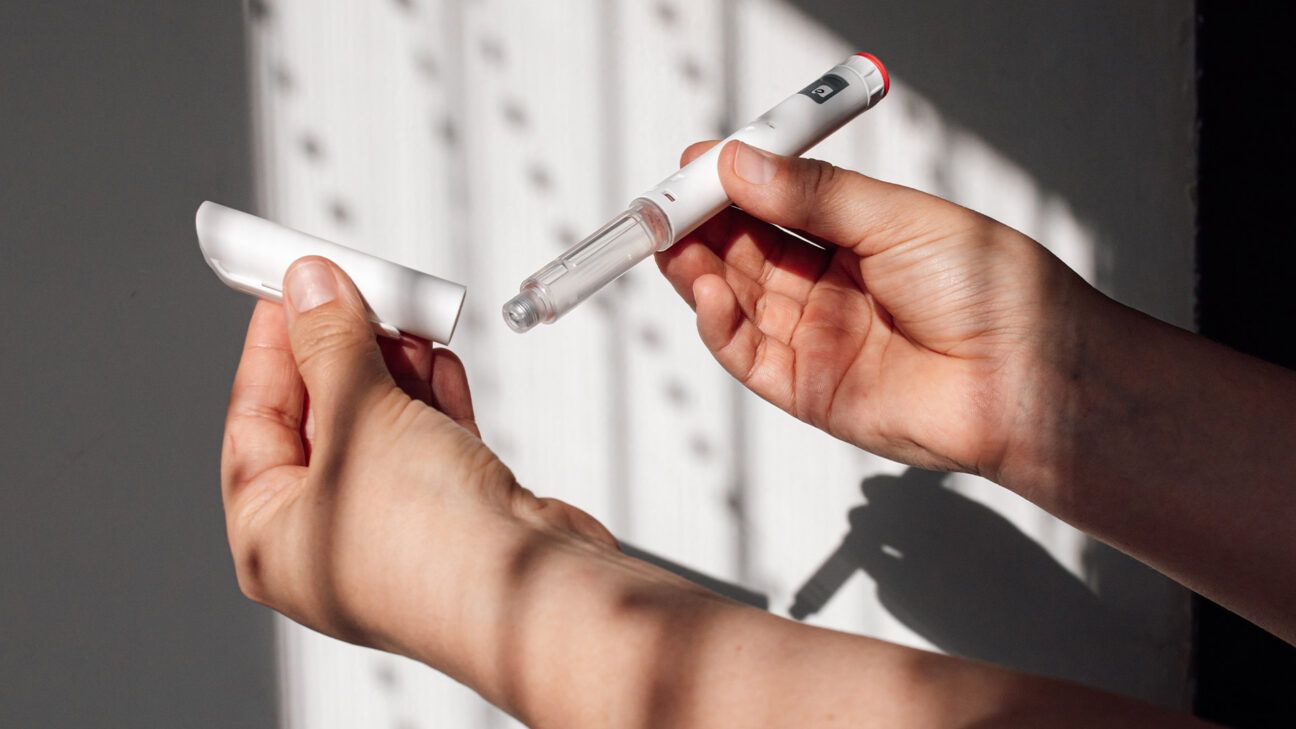
Semaglutide, or Ozempic, is a glucagon-like peptide-1 (GLP-1) agonist. First used as a type 2 diabetes medication, it lowers levels of sugar in the blood.
Semaglutide also reduces appetite and slows digestion, leading to a decrease in food intake and weight loss. Because obesity has been a challenge for many, and so few medications help with weight loss, the drug has taken the world by storm.
Healthline spoke with Mir Ali, MD, a board certified bariatric surgeon and medical director of MemorialCare Surgical Weight Loss Center at Orange Coast Medical Center in Fountain Valley, CA.
“These drugs are more effective than prior available medications in that they directly target hormones that help the patient feel less hungry and more full for a longer period,” he explained.
Obesity: Why taste matters
We are all hardwired to enjoy foods that are high in fat and sugar — these chemicals are the fuel of life. So, when we consume them, our brain “rewards” us with a jolt of pleasure.
In modern Western societies, fat and sugar are much easier to come by than they were thousands of years ago.
Our brains, however, have not yet caught up with the modern food environment and its dizzying array of brightly colored, highly palatable, food and drink.
Accessible at the swipe of a phone screen, we are constantly inundated with opportunities to load up on these delicious, high calorie compounds. Research has found that as we eat more of these foods we may become less sensitive to them, which can be a component for obesity risk.
For instance, previous research showed that people with obesity are less sensitive to sweet tastes, but also more attracted to them. Meanwhile, animal studies have demonstrated that GLP-1 signaling plays a role in taste sensitivity, and sweet taste in particular.
Because of these intriguing relationships, some researchers have wondered whether a change in taste sensitivity might play a role in the weight-loss effects of semaglutide.
Although scientists know that semaglutide mimics hormones that tell the brain you are full, this may not be the only mechanism by which it reduces appetite and drives weight loss.
There is growing evidence that semaglutide and other GLP-1 agonists might also alter how people experience tastes.
How GLP-1 drugs can affect your tastebuds
In the recent study, Sever and colleagues recruited 30 women with obesity and an average age of around 34. Half took semaglutide once weekly, the other took a placebo.
At the beginning and end of the 16-week study, the scientists measured three things:
- Taste sensitivity: Measured using strips impregnated with the four basic tastes — sweet, sour, salty, and bitter.
- Gene expression: By taking biopsies of participants’ tongues.
- Brain responses: Evaluated by a functional MRI scan while a sweet solution dripped onto their tongue before and after a meal.
At the end of the study, the researchers found that those taking semaglutide were more sensitive to tastes than those taking placebo.
According to the abstract, the tongue biopsies showed increased activity of genes associated with “taste signaling transduction pathways, neural plasticity, and renewal of taste buds in the tongue.”
Finally, the brain scans demonstrated that, in response to tasting a sweet solution, there was increased activity in the angular gyrus of the parietal cortex.
This brain region plays a complex role. The angular gyrus combines information from different senses and helps make sense of events or stimuli.
The angular gyrus of the parietal cortex houses GLP-1 receptors and, as the authors of the abstract write, it is part of a “network associated with shifting attention between rewarding and neutral stimuli.”
This change in the angular gyrus might alter an individual’s sensation of the reward linked to sweet tastes. In this way, it could support dietary changes and move the individual toward a healthy weight.
We should note that this is only a proof-of-concept study conducted on a small group of people.
As Sever explains, because the research was carried out in a lab setting, it “may not reflect everyday experience. Taste perception can vary significantly from person to person, limiting the generalizability of our results.”
Who should take semaglutide?
While the weight loss results associated with semaglutide have been impressive, the drug is only suitable for certain people.
Semaglutide has become fashionable in some circles, which is raising concerns with experts. Healthline recently spoke with Federica Amati, PhD, a postdoctoral medical scientist and head nutritionist at ZOE, a science and nutrition company.
“While semaglutide works incredibly well for some people,” explained Amati, who was not involved in the study, “it’s not without its downsides.”
“You should only take it if it has been prescribed to you by a doctor in the context of a multi-disciplinary team that includes psychotherapy, physical activity, and, crucially, dietary advice.”
She explained why eating a good diet is particularly important: Because semaglutide reduces appetite, unless the individual consumes a healthy, diverse diet, there is a danger they might miss out on important nutrients.
“Also, it’s a prescription for life,” Amati continued, “people who come off it tend to regain the weight, so it’s not a quick fix. And more than a third of people experience side effects.”
While most of these side effects are not severe, Amati pointed out they “can be really inconvenient.”
Takeaway
Semaglutide may change the way people perceive sweet tastes.
This may help drive weight loss. However, while effective for many people, semaglutide is not without its drawbacks and should be used with caution.